Transcatheter Aortic Valve Implantation (TAVI)
Aortic stenosis is a disease where the aortic valve has calcium deposits building up on the valve leaflets causing them to be narrowed, rigid and obstructing the blood flow from the heart to the aorta and onward to the rest of the body. This condition makes your heart work harder to pump blood to your body.
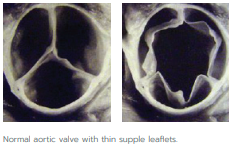

The aortic valve lies between the left ventricle and the aorta and functions by allowing blood to flow in one direction without obstruction.
Traditionally, major open surgery was the only option to replace the aortic valve. Nowadays, the preferred treatment is often the minimally invasive approach called TAVI/TAVR.
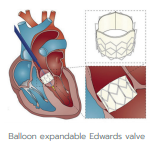
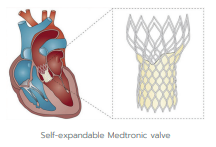
A TAVI is the implantation of an aortic valve without removing the diseased valve, performed under local anaesthesia.
The TAVI approach is X-ray guided and delivers a fully expandable replacement valve to the valve site through a catheter. Once the new valve is expanded, it pushes the old valve leaflets out of the way and the tissue in the replacement valve takes over the normal function of the valve.